Revolutionizing Cataract Treatment with 3D-Printed Implants

Researchers at the University of East Anglia (UEA) are developing a resin that could be used for 3D printing to produce custom-made lenses at lower costs and with increased accessibility.
Recent advancements highlight the potential of 3D printing in ocular applications. Innovations include the development of biodegradable contact lenses, microfluidic chips for drug delivery studies, implants, and a soft hydrogel eye model for testing ocular drug absorption.
You can also read: 3D-Printed Phantom Models for Medical Imaging
Transforming Intraocular Lenses Technology
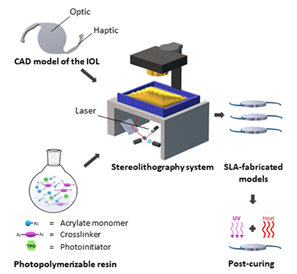
Schematic illustration of the production of lens-like 3D objects without refractive function by stereolithography. Courtesy of: Stereolithographic Rapid Prototyping of Clear, Foldable Non-Refractive Intraocular Lens Designs: A Proof-of-Concept Study.
Intraocular lenses (IOLs) are crucial for people with cataracts, in which the eye’s natural lens becomes cloudy, obscuring vision. Surgeons correct refractive errors like myopia, hyperopia, and presbyopia using intraocular lenses (IOLs).
Dr. Aram Saeed, an Associate Professor in Healthcare Technologies at UEA’s School of Pharmacy, led a team to develop a novel resin for 3D printing ocular devices. With his expertise in material science and healthcare technology, Dr. Saeed highlighted that this innovation enables direct printing of ocular devices. Although in its early stages, this technology has the potential to improve eye care significantly. It offers unprecedented customization and design precision, which could lead to better patient clinical outcomes.
Early Success and Future Directions
In preliminary studies, the researchers demonstrated that the 3D-printed lenses had good optical clarity, could be folded, and were successfully implanted into a human capsular bag. They found no adverse effects on intraocular pressure, electroretinogram, or optical structure, with inflammation markers normalizing within a month.
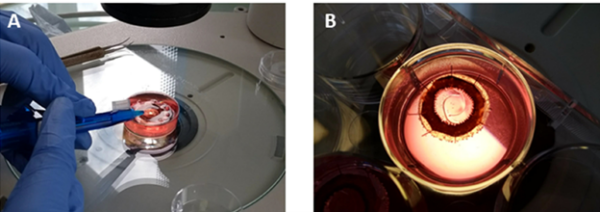
Digital images showing the implantation of a printed IOL-like device in a human capsular bag model in vitro. The delivery of the implant into the capsular bag can be seen in image (A). Once implanted in the capsular bag, the implant recovered its original shape without causing any deformation in this structure (B). Courtesy of : Stereolithographic Rapid Prototyping of Clear, Foldable Non-Refractive Intraocular Lens Designs: A Proof-of-Concept Study.
Co-author Michael Wormstone, Emeritus Professor at UEA’s School of Biological Sciences, emphasized the transformative potential of this technology. “This new technology could enable portable manufacturing solutions, especially beneficial in remote and economically disadvantaged areas,” he said. “It also has the potential to support the production of premium, customized lenses that could enhance surgical outcomes in more advanced healthcare settings.”
Dimensional Accuracy and Thermal Stability
They meticulously measured the printed implants’ dimensions and found 94.5% accuracy for the optical diameter compared to the CAD model. However, they noted the thickness was 64% higher than the theoretical dimension, indicating a need for refinement in the printing process. Additionally, the researchers subjected the printed devices to a post-curing process involving UV irradiation and heating to ensure complete polymerization. This step was crucial to minimize unreacted monomers, thus ensuring biocompatibility and structural integrity.
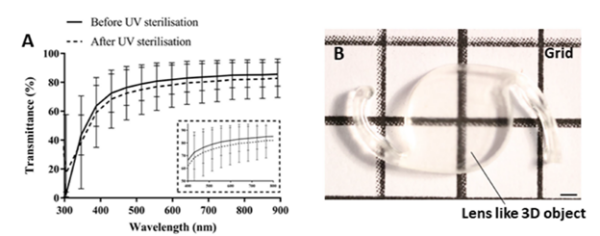
Optical characterization of printed lens-like 3D objects. (a) spectral transmittance of the devices before and after sterilization. A set of implants was sterilized for 1 h with UV irradiation and their light transmittance was compared to non-sterilized counterparts. The spectra indicates that the printed devices allow light transmission within the visible range (380–700 nm) and that the UV sterilization process slightly decreases the light transmittance by ~3%. Courtesy of Stereolithographic Rapid Prototyping of Clear, Foldable Non-Refractive Intraocular Lens Designs: A Proof-of-Concept Study.
Furthermore, they conducted optical characterization of the printed lens-like 3D objects by measuring spectral transmittance before and after sterilization. Specifically, they sterilized a set of implants for 1 hour with UV irradiation and compared their light transmittance to non-sterilized counterparts. The spectra indicated that the printed devices allowed light transmission within the visible range (380–700 nm). However, the UV sterilization process slightly decreased the light transmittance by approximately 3%.
Physico-chemical Properties of 3D-Printed Lenses
The study assessed the physico-chemical properties of the 3D-printed lens-like objects. First, Differential Scanning Calorimetry (DSC) showed that the glass transition temperature (Tg) of the crosslinked polymer was 4.85 ± 1.09 °C. This finding suggests that the material remains flexible at room temperature. Additionally, Thermogravimetric Analysis (TGA) demonstrated that the polymer started to decompose at approximately 382.4 ± 2.17 °C. Therefore, this result indicates good thermal stability for the polymer.
Furthermore, the implants did not absorb water during a one-month incubation in phosphate-buffered saline (PBS) at 35 °C, reflecting their high hydrophobicity. Optical characterization revealed that the implants transmitted 80-85% of visible light, with a slight decrease after UV sterilization. These findings underscore the potential of SLA 3D printing in producing IOLs with desirable optical and mechanical properties, though further optimization is necessary to realize their clinical applicability.
The research has garnered recognition with a United States patent assigned to UEA Enterprise Limited, aiming to commercialize the innovation. The team continues to work closely with industry partners to refine the technology, with hopes of starting clinical trials in the next few years.
To read the full article click here Stereolithographic Rapid Prototyping of Clear, Foldable Non-Refractive Intraocular Lens Designs: A Proof-of-Concept Study.
